RURAL TEENS ARE MORE LIKELY TO SERIOUSLY CONSIDER SUICIDE THAN THEIR URBAN PEERS
Understanding the "Percent of 10th graders who seriously considered suicide" Indicator: To drive meaningful change for kids and families, we rely on data indicators—specific, measurable pieces of information that show how children are doing across key areas like health, education, and economic stability. One indicator of our KIDS COUNT® data project is the rate at which children and youth are considering suicide. The data in this brief specifically looks at 10th graders who responded to the 2023 Healthy Youth Survey. Findings from the data are provided here to help advocates and policymakers assess the severity of one element of the youth behavioral health crisis in our state. View county-level data here.
Overview
Self-report data from the Healthy Youth Survey show that 14% of 10th graders in Washington reported seriously considering suicide in 2023. This is a noticeable decrease from previous years, including an historic high of 23% in 2018, but remains at an unacceptable rate. Much has been done to address the issue of suicidality in youth, and the data shows the start of an optimistic trend in Washington. However, many rural communities continue to report high rates, suggesting that while some efforts to reduce rates of suicidality have made an impact, many communities have been left behind.
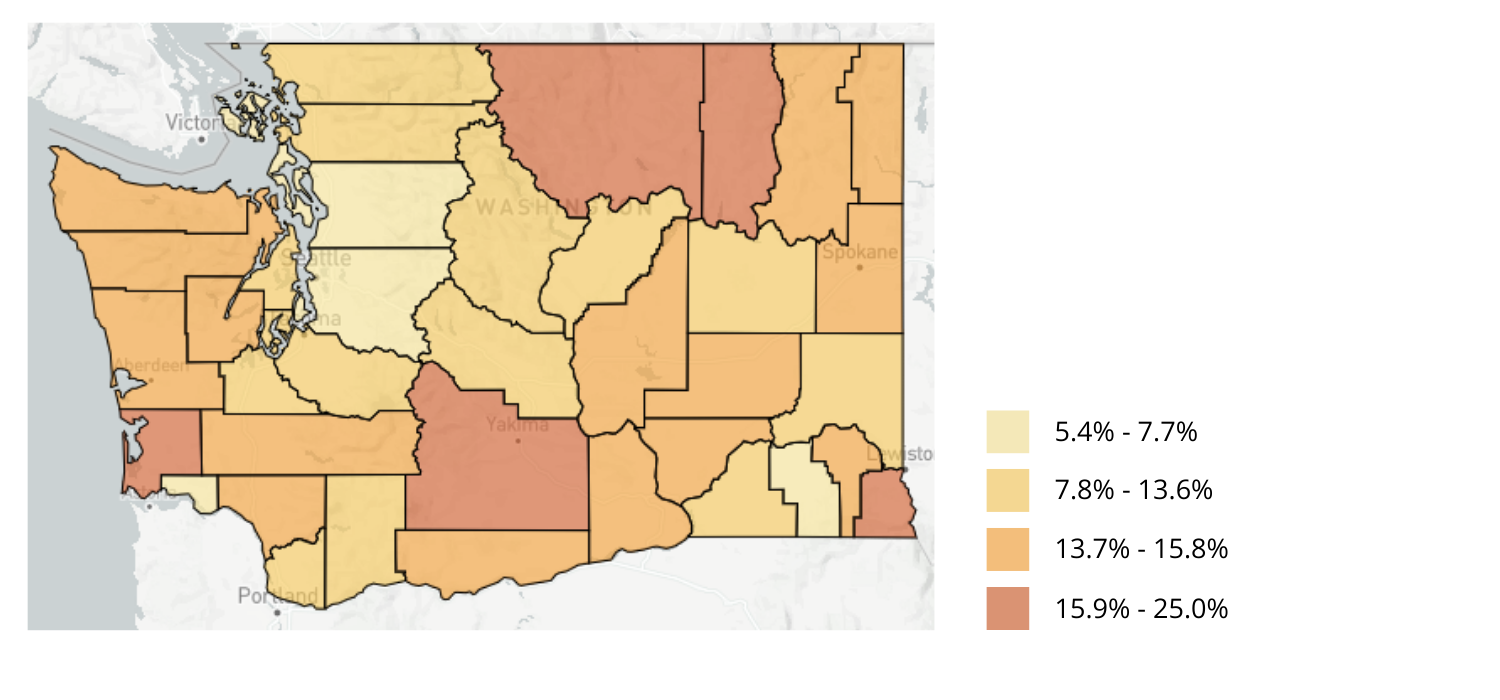
As seen in Image 1, many of the counties where 10th graders are reporting the highest rates of contemplating suicide are rural. For example, Whakiakum County saw the highest rate at 25% of 10th grade respondents reporting to have considered suicide, in contrast with King County, with a rate just under 14%. Across America, rural communities often report higher rates of suicide than their urban counterparts. Research has also shown that suicide rates are increasing faster in rural communities than they are in urban communities. Healthy Youth Survey data suggests this geographic disparity is also true for Washington, where rural counties across the state have some of the highest rates of youth reporting having considered suicide.
Suicidality is not simply an indicator of depression, but of a specific high-acuity mental illness that can stem from untreated major depression, which often occurs alongside other mental illnesses. Suicidality is often indicative of several issues interacting, such as limited access to care and care that does not meet patients’ individual needs. There are also many economic and social determinants that correlate with severe mental illness such as households with limited resources, family makeup, and others. A common thread throughout them all, however, is a lack of access to appropriate care.
An effective youth behavioral health policy solution must account for the difficulty many young people face when searching for care, particularly young people in rural and remote regions. When people have access to clinical interventions, the likelihood of repeated suicide attempts decrease. Increasing access to care is a necessary step in addressing suicidality in young people.
Image 1: Percent of 10th graders who seriously considered suicide by county
Past Work:
Children’s Alliance has previously supported several proposals that aim to increase health equity for rural communities. One example is House Bill 1946, which added behavioral health providers to the list of approved professions for the Washington Health Corps conditional scholarships. This bill, passed in 2024, incentivizes prospective behavioral health providers to serve in under-resourced communities, improving overall access for rural and other underserved populations.
Ongoing Work:
A high priority for Children’s Alliance is developing a diverse and accessible behavioral health workforce. Mental health America reported Washington had a 220:1 ratio of individuals to behavioral health providers in 2024, and a 200:1 ratio in 2025, meaning there has been some improvement in the availability of providers. However, the same reports indicate that the number of youth with major depressive disorder who did not receive treatment remained virtually unchanged in that same period. This may mean that the small growth in the workforce is not yet enough to improve care accessibility, and it is likely that other factors are also at play.
A report commissioned by the Washington State Health Care Authority identified several gaps in services that limit youth access to care in our state, including insufficient supply and uneven distribution of youth inpatient beds, as well as a lack of providers licensed to perform behavioral health assessments and talk-therapy. One especially concerning gap is that only five of the thirty-nine counties in Washington have providers trained in dialectical behavioral therapy, a treatment designed to address extreme emotional dysregulation and reduce self-harm behaviors. This report was commissioned for the express purpose of informing the Washington Thriving Behavioral Health Strategic Plan.
Children’s Alliance is actively collaborating with the authors of the Washington Thriving Behavioral Health Strategic Plan (Plan) to operationalize it over the next several years, focusing on activities that will increase workforce development and improve the continuum of behavioral health care for communities across the state. In partnership with stakeholders and advocates, Children's Alliance is urging the Governor's adoption of the Plan at the state level and will continue to work with partners to ensure implementation.
———
Data Sources:
The data used for this measure come from the 2023 Washington State Healthy Youth Survey (HYS). Data were retrieved in June 2024 from: http://www.askhys.net/.
KIDS COUNT® is a registered trademark of The Annie E. Casey Foundation., Inc., and is used with permission of the Foundation.